Public Health is a Job for Engineers
Public Health is a Job for Engineers


Physicians can cure diseases, but mechanical engineers build defenses to ward off pathogens before they infect.
In the winter months of 2021, after a grueling year of pandemic and its associated disruptions, there was no news as welcome as the roll out of various vaccines against COVID-19. First with the most vulnerable as well as essential workers and then through the rest of the population, the vaccines were seen as the beginning of the end of the pandemic, at least in the United States where they were most readily available. Medical science had triumphed.
This hopeful and popular story hides an important point: The COVID-19 pandemic occurred due to a failure to apply good engineering to the cause of public health.
The vaccines employed to stop COVID create defenses against the virus within the human body. They don’t stop infection entirely, but instead fight its ability to cause disease and even then, do so imperfectly. (The number of so-called breakthrough cases among fully vaccinated people is small compared to the rate of disease in unvaccinated populations, but it is still significant.)
What’s more, relying on vaccines as the main tool to stop new airborne diseases will inevitably result in large numbers of deaths, since viruses do not send advance notice that they are coming so we can begin vaccine development. We were lucky this time because COVID is not as deadly as other diseases—pandemics in history have killed large fractions of the population—and effective vaccines were developed with amazing speed. The next pathogen may not be so kind, and coupled with an inevitable return to global air travel and the human desire to crowd into bars, restaurants, arenas, offices, and other confined spaces, will result in another pandemic overtaking the globe.
There is another way. Instead of waiting to fight diseases inside the human body, engineering can establish lines of defense further out by either intercepting and neutralizing the pathogens before they reach humans or diluting them so much that they can’t build up an infective load. Good engineering can create robust public health.
In fact, mechanical engineers have been responsible for many of the most significant advances in health. The cholera and dysentery epidemics of history were stopped by water and sewer systems that prevented transmission of those waterborne diseases. Malaria has been eliminated in many places through use of window screens and the killing of the parasite-bearing mosquitoes. Food-borne illnesses have been greatly reduced by advances in cooking, packing, and freezing technology.
The engineering solutions that stopped transmission of diseases by water, insects, and food brought about the largest increases in life expectancies in human history. Most of those advances occurred in the last half of the 19th century and the first half of the 20th century. To be sure, none of those diseases have been eliminated entirely, but the job by engineers in erecting defenses is so effective that the medical science community—physicians and the developers of vaccines and other treatments—are the backup squad.
Engineering Against COVID: 2020 Emerging Technology Awards
With those successes it appeared that it was only a matter of time before safe air would follow safe water. However, in the 1960s with the early success of some vaccines, the medical science community took over public health and implemented a major change in strategy. Instead of preventing disease transmission to and between people, the idea was to use vaccines so individuals may get infected but not get sick.
Vaccines have been successful against individual diseases; they have triumphed over the scourges of smallpox and polio, for instance. But the emergence of the novel coronavirus in 2019 should prompt us to revisit that reactive stance. It is time to examine how good mechanical engineering can stop transmission of all airborne diseases.
In the United States each year, about 3,000 people die of food poisoning and about 6,000 people die from contaminated water. This compares to the situation in the 19th century, when contaminated food and water killed hundreds of thousands of people in the U.S. annually, and from a much smaller population base. This success is due to public health measures based on engineering. A vaccine or medical treatment might only prove effective against a single strain of organism, and waterborne illnesses are caused by 17 different pathogens; water treatment plants are effective against every one of them. Similarly, non-medical interventions are effective against a whole range of disease-causing organisms in food.
Another success in health and safety is found in the fight against urban fires. In the 1800s, rapid urbanization and shoddy wood construction led to great fires that burned down large portions of many cities, including New York, St. Louis, Boston, and famously Chicago. The way the fires spread across the cities, jumping from one building to the next, was analogous to a pandemic. And in that analogy, fire departments are the equivalent of the medical profession to diseases—perhaps able to save single buildings but incapable of stopping the rapidly spreading fires. Often, the fires died out once they had consumed all available buildings.
The solution to the great fire epidemic was building codes that required new construction to be made from brick, concrete, stone, and plaster—all fire-resistant materials. The solution did not stop an occasional building from burning to the ground, but raging, city-wide fires were a thing of the past.
While engineered solutions have had great success in these areas of public health, the strategy has hardly been tried to fight airborne diseases. The death toll from these pathogens has been steep: In a normal year in the United States, 20,000 to 30,000 people die from influenza. And the number of U.S. deaths attributed to COVID-19 reached 825,000 by the end of 2021 and could approach 1 million before the pandemic is over. Worldwide, estimates for the death toll from COVID-19 range from 5 million to more than 15 million.
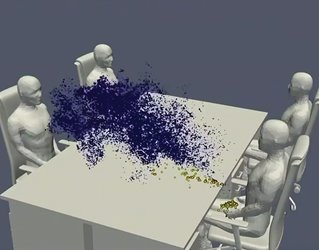
The engineering paradigm to fighting airborne diseases would be to stop local transmission of the disease—providing clean air the way engineered systems supply clean water. It is not necessary to clean all air to stop airborne pandemics, just air where many people are crowded together to keep the disease transmission rate below one new infection for each person with the virus.
The implication is that some will get sick and need medical treatment, a few will even die, but the engineering strategy of providing safe air prevents these diseases from developing into pandemics.
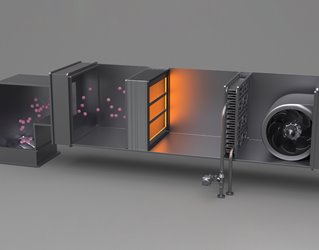
The public health engineering approach to fighting airborne diseases would have two major components. The first is the use of filters to clear the air of pathogens and prevent the transmission of diseases between people.
For decades there has been an ongoing debate in the heating and ventilation community between energy efficiency and air quality. Sealing buildings to prevent air infiltration reduces heating and cooling bills and is thus attractive to building owners, who foot utility costs. Others who have studied the effects of these sealed buildings contend that better quality air in buildings and other public places would save more money through better worker productivity. Even in non-pandemic times, workers in sealed buildings tend to spread cold and flu germs to their colleagues. In addition to sick days taken due to influenza and other airborne diseases, there are massive amounts of low productivity from moderately sick workers dragging themselves into the office.
This was shrugged off as a normal state of affairs, but during the pandemic it was shown that the flu could be stopped. The isolation and masks used to fight COVID broke the chain of transmission for other airborne diseases as well and reduced U.S. flu deaths to less than a 1,000 during the 2020-2021 flu season.
The evidence is piling up that safe air where viruses have been filtered out or destroyed is cheaper than deaths, lost work time, and lower productivity—separate from protection against pandemics. There are several paths to cleaning the air from pathogens, including placing filters in the ventilation system or exposing the circulating air to virus-destroying UV light, but they have clear advantages over medical interventions. Air cleaning works against all air-borne viruses, does not require knowing which viruses are in circulation, and does not depend upon convincing or forcing everyone to be vaccinated or wear masks.
I know of industrial companies, schools, hotels (and even my dentist) that have adopted this strategy. The cost of clean, filtered air is small wherever buildings have the space—all that is needed are simple, cheap filter and fan systems. Even the tight quarters of aircraft should be easy to adapt, since commercial aircraft ventilation systems today have filters that remove viruses, so only small changes in air distribution are needed to minimize mixing air between passengers and disease transmission. The cost to improve air distribution systems with new aircraft or when replacing the interiors of old aircraft will be close to zero.
More on Public Health: Biofuel Made in New York
The challenges will be in dense, urban areas. Transit will be expensive to bring into line, as subway cars have limited space to install safe, filtered air systems without cutting off the top half of the car to provide space for equipment or using up significant passenger space. The cost in new buildings is low, but retrofitting will be expensive in some historic buildings constructed when public health was either ignored or not a priority. In cities like New York where the oldest apartment buildings were built without thought to electricity or running water, adding clean air systems will be a struggle. That’s also the case for ultramodern, energy-efficient buildings that recycle air with low-grade filters to reduce energy costs of heating, cooling, and reducing the humidity of outside air. We have unintentionally engineered into many buildings and mass transit the easy transmission of airborne diseases between people.
Another public health engineering solution is sensors that could enable everyone to know if they are in a location with a high risk of spreading airborne viruses from one person to another. During the pandemic, many health agencies released smartphone apps that alert users if they have been in areas where infected people have been, but that is by necessity an after-the-fact notification. It is possible through engineering to provide immediate notice of potentially hazardous conditions.
When you exhale, you expel both carbon dioxide and microbes such as viruses and bacteria that line your lungs and respiratory tract. The more people in your vicinity, the higher the carbon dioxide content in the air—and more likely than not, the higher the pathogen load. Cheap carbon dioxide detectors installed in indoor public locations could read out CO2 levels and send that information to nearby cell phones. It isn’t a direct detection of viruses but should be a good proxy. And what’s more, because it isn’t tuned to any specific disease, it would provide a warning that is effective against all airborne viruses and bacteria. The more carbon dioxide in the air, the higher the chance pathogens are floating in it.
Some organizations today use such detectors to protect employees against COVID-19. If carbon dioxide levels reach a certain point, employees are instructed to open windows or even go home early for safety. In addition to smartphone notifications, it’s easy to envision a requirement for real-time air-quality data to be posted on the front doors of trains, buses, bars, high school auditoriums—basically anywhere large numbers of people might crowd together in potential superspreader events.
A requirement for carbon dioxide monitors with cell phone readout and signs on the front doors would have three impacts. Carbon-dioxide air monitors would provide a guidance on where clean air systems are required beyond the obvious locations. Second, consumers would likely demand businesses install clean air systems if they were consistently crowded, forcing the hands of owners who might want to avoid the cost.
Finally, in the case of a future airborne pandemic, public health officials could limit the closure of businesses and public spaces to those that have demonstrated build-ups of exhaled air, rather than every business in a jurisdiction. In this way, the use of mechanical engineering in public health would provide cost-effective disease prevention.
Historically, most epidemics were local and quickly died out. Even at the turn of this century, transport networks had large enough gaps that if a new disease appeared in rural Asia or Africa, it could be difficult for it to be carried to a large city. Today, the global air transportation system connects much of the world at a more granular level, and large metropolises are found everywhere. (According to United Nations estimates, there were 33 metropolitan areas with more than 10 million people in 2018, and only five were in G7 nations.) These connections make it seem unlikely that COVID-19 will be the only pandemic we see in the first half of the 21st century.
Engineering Solutions: Recycling Desalination Waste
The public health responses to COVID-19 over the past two years have been based on the faith that this coronavirus is a one-time, short-term event, and that after a period of lockdowns and facemasks, vaccines will bring about a return to normal. This faith is, in fact, historical amnesia. History has shown that most diseases are stopped by shutting down disease transmission, not late-arriving vaccines or hospital treatments, and that the most enduring way to stop transmission is via engineered public health systems such as water treatment plants and mosquito control districts.
Safe air, provided by technologies developed and implemented by mechanical engineers, will stop COVID-19 and its mutations, as well as colds, flus, and other airborne diseases. But first we will have to make a conscious decision to build them.
Charles W. Forsberg is a principal research scientist in the Department Nuclear Science and Engineering at the Massachusetts Institute of Technology in Cambridge and principal investigator of the DOE Integrated Research Project on Fluoride-Salt-Cooled High-Temperature Reactors.
This hopeful and popular story hides an important point: The COVID-19 pandemic occurred due to a failure to apply good engineering to the cause of public health.
The vaccines employed to stop COVID create defenses against the virus within the human body. They don’t stop infection entirely, but instead fight its ability to cause disease and even then, do so imperfectly. (The number of so-called breakthrough cases among fully vaccinated people is small compared to the rate of disease in unvaccinated populations, but it is still significant.)
What’s more, relying on vaccines as the main tool to stop new airborne diseases will inevitably result in large numbers of deaths, since viruses do not send advance notice that they are coming so we can begin vaccine development. We were lucky this time because COVID is not as deadly as other diseases—pandemics in history have killed large fractions of the population—and effective vaccines were developed with amazing speed. The next pathogen may not be so kind, and coupled with an inevitable return to global air travel and the human desire to crowd into bars, restaurants, arenas, offices, and other confined spaces, will result in another pandemic overtaking the globe.
There is another way. Instead of waiting to fight diseases inside the human body, engineering can establish lines of defense further out by either intercepting and neutralizing the pathogens before they reach humans or diluting them so much that they can’t build up an infective load. Good engineering can create robust public health.
In fact, mechanical engineers have been responsible for many of the most significant advances in health. The cholera and dysentery epidemics of history were stopped by water and sewer systems that prevented transmission of those waterborne diseases. Malaria has been eliminated in many places through use of window screens and the killing of the parasite-bearing mosquitoes. Food-borne illnesses have been greatly reduced by advances in cooking, packing, and freezing technology.
The engineering solutions that stopped transmission of diseases by water, insects, and food brought about the largest increases in life expectancies in human history. Most of those advances occurred in the last half of the 19th century and the first half of the 20th century. To be sure, none of those diseases have been eliminated entirely, but the job by engineers in erecting defenses is so effective that the medical science community—physicians and the developers of vaccines and other treatments—are the backup squad.
Engineering Against COVID: 2020 Emerging Technology Awards
With those successes it appeared that it was only a matter of time before safe air would follow safe water. However, in the 1960s with the early success of some vaccines, the medical science community took over public health and implemented a major change in strategy. Instead of preventing disease transmission to and between people, the idea was to use vaccines so individuals may get infected but not get sick.
Vaccines have been successful against individual diseases; they have triumphed over the scourges of smallpox and polio, for instance. But the emergence of the novel coronavirus in 2019 should prompt us to revisit that reactive stance. It is time to examine how good mechanical engineering can stop transmission of all airborne diseases.
Nonmedical Interventions
In the United States each year, about 3,000 people die of food poisoning and about 6,000 people die from contaminated water. This compares to the situation in the 19th century, when contaminated food and water killed hundreds of thousands of people in the U.S. annually, and from a much smaller population base. This success is due to public health measures based on engineering. A vaccine or medical treatment might only prove effective against a single strain of organism, and waterborne illnesses are caused by 17 different pathogens; water treatment plants are effective against every one of them. Similarly, non-medical interventions are effective against a whole range of disease-causing organisms in food.
Another success in health and safety is found in the fight against urban fires. In the 1800s, rapid urbanization and shoddy wood construction led to great fires that burned down large portions of many cities, including New York, St. Louis, Boston, and famously Chicago. The way the fires spread across the cities, jumping from one building to the next, was analogous to a pandemic. And in that analogy, fire departments are the equivalent of the medical profession to diseases—perhaps able to save single buildings but incapable of stopping the rapidly spreading fires. Often, the fires died out once they had consumed all available buildings.
The solution to the great fire epidemic was building codes that required new construction to be made from brick, concrete, stone, and plaster—all fire-resistant materials. The solution did not stop an occasional building from burning to the ground, but raging, city-wide fires were a thing of the past.
While engineered solutions have had great success in these areas of public health, the strategy has hardly been tried to fight airborne diseases. The death toll from these pathogens has been steep: In a normal year in the United States, 20,000 to 30,000 people die from influenza. And the number of U.S. deaths attributed to COVID-19 reached 825,000 by the end of 2021 and could approach 1 million before the pandemic is over. Worldwide, estimates for the death toll from COVID-19 range from 5 million to more than 15 million.
The engineering paradigm to fighting airborne diseases would be to stop local transmission of the disease—providing clean air the way engineered systems supply clean water. It is not necessary to clean all air to stop airborne pandemics, just air where many people are crowded together to keep the disease transmission rate below one new infection for each person with the virus.
The implication is that some will get sick and need medical treatment, a few will even die, but the engineering strategy of providing safe air prevents these diseases from developing into pandemics.
Engineering Safe Air
The public health engineering approach to fighting airborne diseases would have two major components. The first is the use of filters to clear the air of pathogens and prevent the transmission of diseases between people.
For decades there has been an ongoing debate in the heating and ventilation community between energy efficiency and air quality. Sealing buildings to prevent air infiltration reduces heating and cooling bills and is thus attractive to building owners, who foot utility costs. Others who have studied the effects of these sealed buildings contend that better quality air in buildings and other public places would save more money through better worker productivity. Even in non-pandemic times, workers in sealed buildings tend to spread cold and flu germs to their colleagues. In addition to sick days taken due to influenza and other airborne diseases, there are massive amounts of low productivity from moderately sick workers dragging themselves into the office.
This was shrugged off as a normal state of affairs, but during the pandemic it was shown that the flu could be stopped. The isolation and masks used to fight COVID broke the chain of transmission for other airborne diseases as well and reduced U.S. flu deaths to less than a 1,000 during the 2020-2021 flu season.
The evidence is piling up that safe air where viruses have been filtered out or destroyed is cheaper than deaths, lost work time, and lower productivity—separate from protection against pandemics. There are several paths to cleaning the air from pathogens, including placing filters in the ventilation system or exposing the circulating air to virus-destroying UV light, but they have clear advantages over medical interventions. Air cleaning works against all air-borne viruses, does not require knowing which viruses are in circulation, and does not depend upon convincing or forcing everyone to be vaccinated or wear masks.
I know of industrial companies, schools, hotels (and even my dentist) that have adopted this strategy. The cost of clean, filtered air is small wherever buildings have the space—all that is needed are simple, cheap filter and fan systems. Even the tight quarters of aircraft should be easy to adapt, since commercial aircraft ventilation systems today have filters that remove viruses, so only small changes in air distribution are needed to minimize mixing air between passengers and disease transmission. The cost to improve air distribution systems with new aircraft or when replacing the interiors of old aircraft will be close to zero.
More on Public Health: Biofuel Made in New York
The challenges will be in dense, urban areas. Transit will be expensive to bring into line, as subway cars have limited space to install safe, filtered air systems without cutting off the top half of the car to provide space for equipment or using up significant passenger space. The cost in new buildings is low, but retrofitting will be expensive in some historic buildings constructed when public health was either ignored or not a priority. In cities like New York where the oldest apartment buildings were built without thought to electricity or running water, adding clean air systems will be a struggle. That’s also the case for ultramodern, energy-efficient buildings that recycle air with low-grade filters to reduce energy costs of heating, cooling, and reducing the humidity of outside air. We have unintentionally engineered into many buildings and mass transit the easy transmission of airborne diseases between people.
Another public health engineering solution is sensors that could enable everyone to know if they are in a location with a high risk of spreading airborne viruses from one person to another. During the pandemic, many health agencies released smartphone apps that alert users if they have been in areas where infected people have been, but that is by necessity an after-the-fact notification. It is possible through engineering to provide immediate notice of potentially hazardous conditions.
When you exhale, you expel both carbon dioxide and microbes such as viruses and bacteria that line your lungs and respiratory tract. The more people in your vicinity, the higher the carbon dioxide content in the air—and more likely than not, the higher the pathogen load. Cheap carbon dioxide detectors installed in indoor public locations could read out CO2 levels and send that information to nearby cell phones. It isn’t a direct detection of viruses but should be a good proxy. And what’s more, because it isn’t tuned to any specific disease, it would provide a warning that is effective against all airborne viruses and bacteria. The more carbon dioxide in the air, the higher the chance pathogens are floating in it.
Some organizations today use such detectors to protect employees against COVID-19. If carbon dioxide levels reach a certain point, employees are instructed to open windows or even go home early for safety. In addition to smartphone notifications, it’s easy to envision a requirement for real-time air-quality data to be posted on the front doors of trains, buses, bars, high school auditoriums—basically anywhere large numbers of people might crowd together in potential superspreader events.
A requirement for carbon dioxide monitors with cell phone readout and signs on the front doors would have three impacts. Carbon-dioxide air monitors would provide a guidance on where clean air systems are required beyond the obvious locations. Second, consumers would likely demand businesses install clean air systems if they were consistently crowded, forcing the hands of owners who might want to avoid the cost.
Finally, in the case of a future airborne pandemic, public health officials could limit the closure of businesses and public spaces to those that have demonstrated build-ups of exhaled air, rather than every business in a jurisdiction. In this way, the use of mechanical engineering in public health would provide cost-effective disease prevention.
Scalable Solutions
Historically, most epidemics were local and quickly died out. Even at the turn of this century, transport networks had large enough gaps that if a new disease appeared in rural Asia or Africa, it could be difficult for it to be carried to a large city. Today, the global air transportation system connects much of the world at a more granular level, and large metropolises are found everywhere. (According to United Nations estimates, there were 33 metropolitan areas with more than 10 million people in 2018, and only five were in G7 nations.) These connections make it seem unlikely that COVID-19 will be the only pandemic we see in the first half of the 21st century.
Engineering Solutions: Recycling Desalination Waste
The public health responses to COVID-19 over the past two years have been based on the faith that this coronavirus is a one-time, short-term event, and that after a period of lockdowns and facemasks, vaccines will bring about a return to normal. This faith is, in fact, historical amnesia. History has shown that most diseases are stopped by shutting down disease transmission, not late-arriving vaccines or hospital treatments, and that the most enduring way to stop transmission is via engineered public health systems such as water treatment plants and mosquito control districts.
Safe air, provided by technologies developed and implemented by mechanical engineers, will stop COVID-19 and its mutations, as well as colds, flus, and other airborne diseases. But first we will have to make a conscious decision to build them.
Charles W. Forsberg is a principal research scientist in the Department Nuclear Science and Engineering at the Massachusetts Institute of Technology in Cambridge and principal investigator of the DOE Integrated Research Project on Fluoride-Salt-Cooled High-Temperature Reactors.