Treating Pain without Drugs: Implantable Device Cools Nerves
Treating Pain without Drugs: Implantable Device Cools Nerves
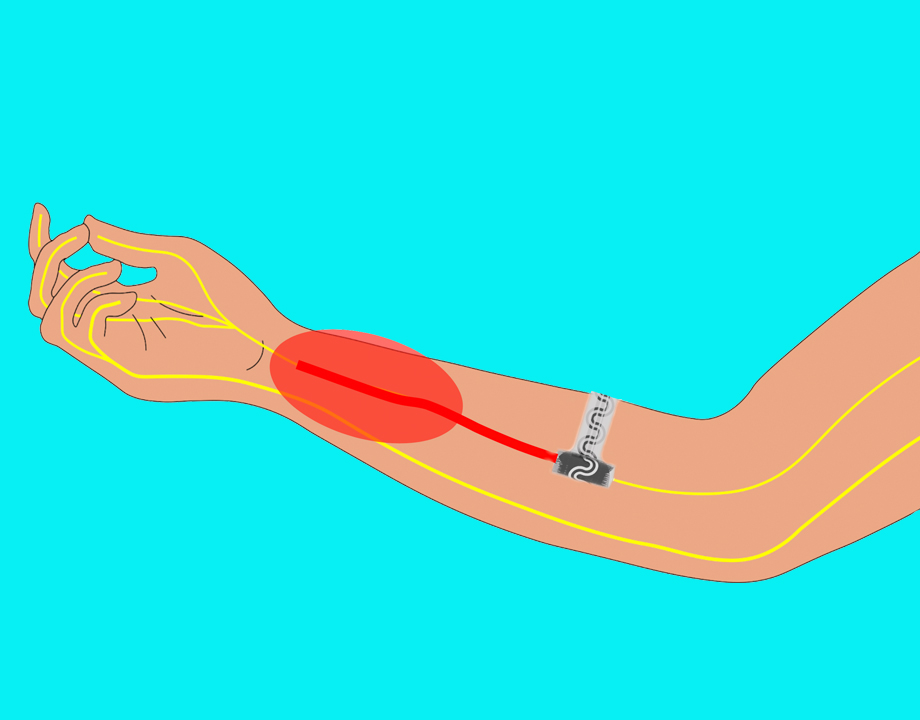
Pump sends coolant to device wrapped around nerve to numb and block pain signals. Image: Northwestern University
With the ongoing concerns of the addictive nature of opiates and dangerous risks of other pain medications, many medical practioners are at a loss on how to help patients experiencing pain. This prominent gap in care has inspired a group of researchers at Northwestern University to develop a pain-relieving device that could be implanted after a surgery.
John A. Rogers, whose lab is developing the device, said targeting pain at the source has always been a challenge. Medications may relieve the pain, but because it isn’t localized, there are many potential side effects. Injections can also work to an extent, but aren’t localized enough and may cause damage and inflammation to the surrounding tissue. But with this device, relief would be provided at the source with no greater impact on the rest of the body.
“In some cases, you really need devices inside the body,” he said. “The goal is for the device to provide relief and then dissolve and disappear to eliminate the threat from a secondary surgical extraction.”
The device would be placed and loosely wrapped around the affected nerve, where it would deliver targeted and precise cooling to numb the nerve and block pain signals. An external pump allows the user to activate and adjust the cooling level. Once the patient is healed and the device is no longer needed, it would simply dissolve in the body over time, much like internal sutures do.
Rogers, the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering, and Neurological Surgery, said the device is made of a watersoluble material that is thin and flexible. It looks very much like a rubber band and is about five millimeters wide. It is interlayed with a serpentine-shaped microfluidic channel, which is filled with coolant.
More for You: Identifying Gastric Disease from the Inside
The coolant is a low-boiling-point liquid used in other medical applications such as inhalers and as an intravenous ultrasound contrast enhancement material. Once inside the body, its temperature is higher than its boiling point. Rogers said the liquid wants to begin to evaporate, but cannot until the fluid travels down the device and encounters a separate stream of nitrogen that is introduced through a parallel channel at the position of the cuff. When the liquid evaporates and enters a gaseous state, it pulls heat from the nerve and thereby provides targeted cooling power.
Excessive cooling can damage the nerve and the surrounding tissue. To address that, a small sensor within the device monitors the temperature of the nerve, which is displayed on the external pump. Based off this temperature reading, the cooling power can be dialed to various degrees of strength and switched on and off.
“There's really no other cooling going on,” Rogers noted. “It's just right at the location of that nerve, so you're not parasitically cooling surrounding tissue.”
The work is described in a paper recently published in Science. ”The technology reported here exploits mechanisms that have some similarities to those that cause your fingers to feel numb when cold,” said Rogers.
Reader’s Choice: Renewed Mensicus
In addition to controlling the level of cooling, the team was also challenged with finding materials that would not damage the fragile nerve or any surrounding tissue. They had to be very soft and compliant, and resorb quickly enough so not to cause any adverse impacts on the patient.
“Building the device out of bio-resorbable materials was a critical advance because as you might imagine, if the device doesn't resorb, then the body might reject it and create scar tissue, making it difficult to extract and cause more pain for the patient,” he said.
So far, the team has had success testing the device in animal trials, but they want to further explore the long-term impact of direct cooling on the nerves and whether to refine the temperature and duration settings of the device. It may take up to 10 years to complete trials and receive FDA approval.
As Rogers and his team continue to develop devices for the medical community, including a dissolvable pacemaker, it remains important that they work in tandem with those who understand the human body best.
“We strive to develop new materials, new types of devices, that could improve patient care, either by reducing costs or improving outcomes,” he said. “I think to be effective with this sort of work, it requires a deep, intimate kind of collaborative engagement with not only the physicians and the clinicians, but also the nurses and the caregivers to understand where the most pressing unmet needs are and how advances in technology may address those needs.”
Cassandra Martindell writes about science and technology from Columbus, Ohio.
John A. Rogers, whose lab is developing the device, said targeting pain at the source has always been a challenge. Medications may relieve the pain, but because it isn’t localized, there are many potential side effects. Injections can also work to an extent, but aren’t localized enough and may cause damage and inflammation to the surrounding tissue. But with this device, relief would be provided at the source with no greater impact on the rest of the body.
“In some cases, you really need devices inside the body,” he said. “The goal is for the device to provide relief and then dissolve and disappear to eliminate the threat from a secondary surgical extraction.”
The device would be placed and loosely wrapped around the affected nerve, where it would deliver targeted and precise cooling to numb the nerve and block pain signals. An external pump allows the user to activate and adjust the cooling level. Once the patient is healed and the device is no longer needed, it would simply dissolve in the body over time, much like internal sutures do.
Rogers, the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering, and Neurological Surgery, said the device is made of a watersoluble material that is thin and flexible. It looks very much like a rubber band and is about five millimeters wide. It is interlayed with a serpentine-shaped microfluidic channel, which is filled with coolant.
More for You: Identifying Gastric Disease from the Inside
The coolant is a low-boiling-point liquid used in other medical applications such as inhalers and as an intravenous ultrasound contrast enhancement material. Once inside the body, its temperature is higher than its boiling point. Rogers said the liquid wants to begin to evaporate, but cannot until the fluid travels down the device and encounters a separate stream of nitrogen that is introduced through a parallel channel at the position of the cuff. When the liquid evaporates and enters a gaseous state, it pulls heat from the nerve and thereby provides targeted cooling power.
Excessive cooling can damage the nerve and the surrounding tissue. To address that, a small sensor within the device monitors the temperature of the nerve, which is displayed on the external pump. Based off this temperature reading, the cooling power can be dialed to various degrees of strength and switched on and off.
“There's really no other cooling going on,” Rogers noted. “It's just right at the location of that nerve, so you're not parasitically cooling surrounding tissue.”
The work is described in a paper recently published in Science. ”The technology reported here exploits mechanisms that have some similarities to those that cause your fingers to feel numb when cold,” said Rogers.
Reader’s Choice: Renewed Mensicus
In addition to controlling the level of cooling, the team was also challenged with finding materials that would not damage the fragile nerve or any surrounding tissue. They had to be very soft and compliant, and resorb quickly enough so not to cause any adverse impacts on the patient.
“Building the device out of bio-resorbable materials was a critical advance because as you might imagine, if the device doesn't resorb, then the body might reject it and create scar tissue, making it difficult to extract and cause more pain for the patient,” he said.
So far, the team has had success testing the device in animal trials, but they want to further explore the long-term impact of direct cooling on the nerves and whether to refine the temperature and duration settings of the device. It may take up to 10 years to complete trials and receive FDA approval.
As Rogers and his team continue to develop devices for the medical community, including a dissolvable pacemaker, it remains important that they work in tandem with those who understand the human body best.
“We strive to develop new materials, new types of devices, that could improve patient care, either by reducing costs or improving outcomes,” he said. “I think to be effective with this sort of work, it requires a deep, intimate kind of collaborative engagement with not only the physicians and the clinicians, but also the nurses and the caregivers to understand where the most pressing unmet needs are and how advances in technology may address those needs.”
Cassandra Martindell writes about science and technology from Columbus, Ohio.





.png?width=854&height=480&ext=.png)
