3D Printing Living Skin with Blood Vessels
3D Printing Living Skin with Blood Vessels
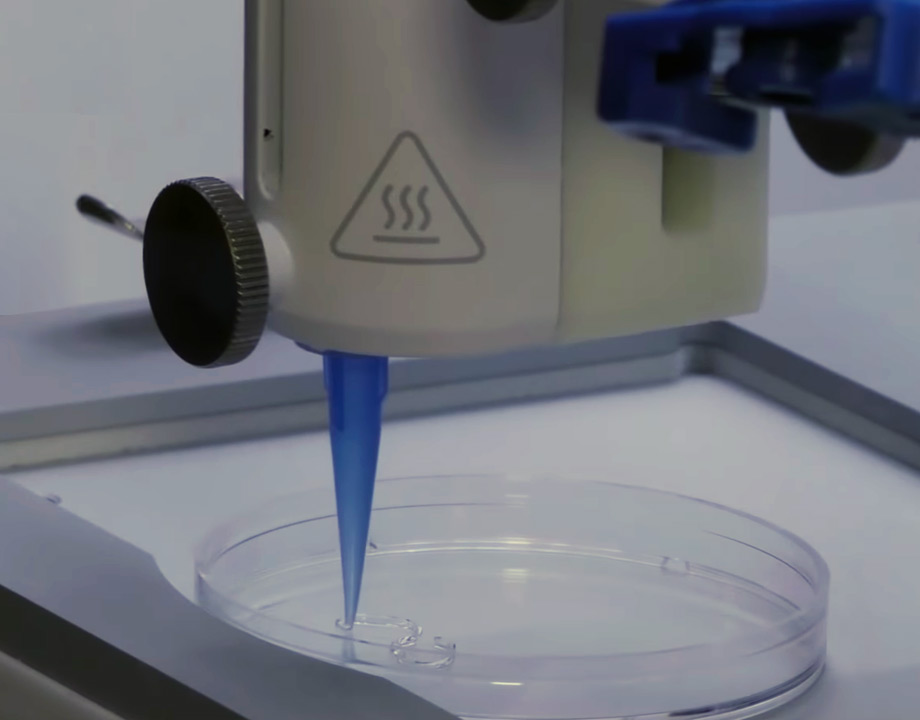
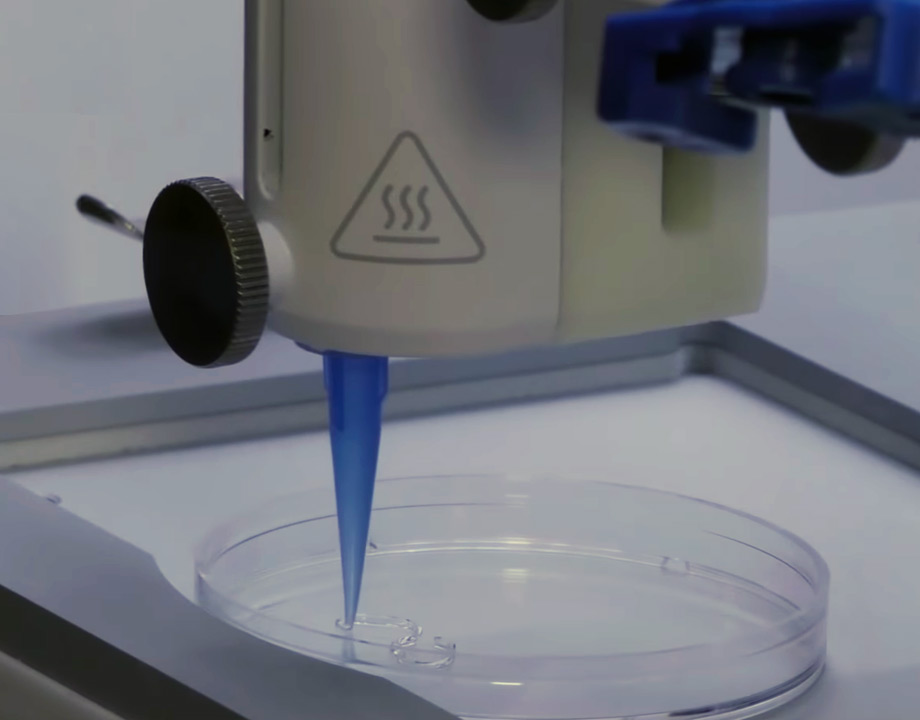
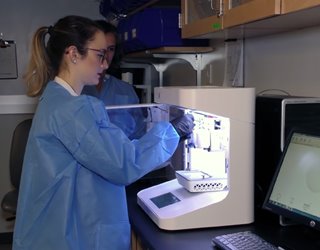
Bioengineers developed a way to incorporate blood vessels into 3D-printed living skin. Photo: Rensselaer Polytechnic Institute
Step by step, Pankaj Karande has made steady progress in creating skin grafts that are much closer to what the human body itself produces and more likely to be integrated and accepted by a patient’s body.
In the most recent development discussed in an article in Tissue Engineering, Karande, an associate professor of chemical and biological engineering at Rensselaer Polytechnic Institute, and the team in his lab at Rensselaer, collaborating with Yale School of Medicine, have developed a way to use 3D printing to incorporate blood vessels into the living skin they produce. “That was a big breakthrough,” Karande said.
Within the past decade, 3D bioprinting has actually played a starring role in advancing the field of skin engineering. Karande published one of the first papers in the field showing that researchers could make a bio-ink from two types of living human cells and use a 3D printer to produce a skin-like structure. The traditional procedure for making skin was to take cells, mix them up with collagen, and spread them in thin layers.
“You might liken it to spreading jam on a piece of bread in layers,” he said, adding that it’s very hard to do so manually, because you are working with tens or hundreds of microns that need to be close to the other cells for normal interaction.
You May Also Like: Artificial and 3D-Printed Skin Advances for Robots, Humans
3D printing has allowed precise placement and arrangement of the cells in three dimensions on a very small scale—this material that can be 10 times thinner than a human hair. “That’s been the big advancement that 3D printing has allowed in soft tissue engineering,” Karande said.
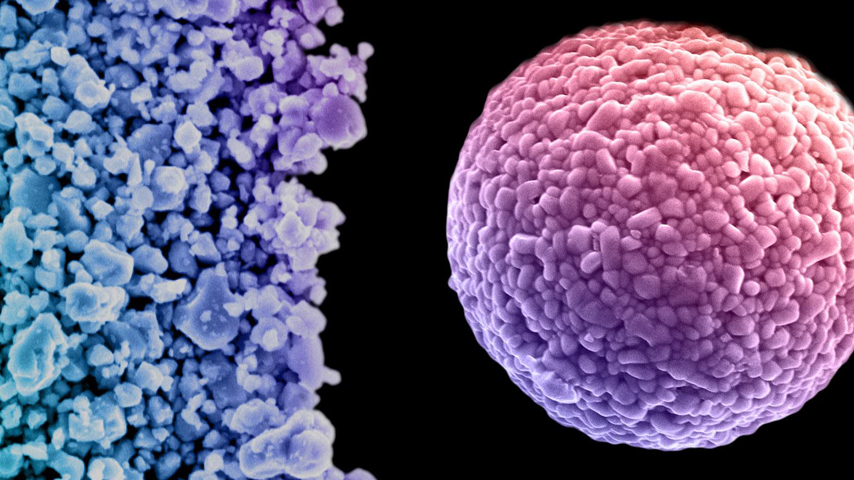
Although this was a “big advancement,” a few years ago the team realized that for the grafts to survive on patients, blood vessels are very critical. At that time a lot of work was being done on combining endothelial and other cells to try to form blood vessels, but the available methods weren’t working.
Karande’s team decided to try putting cells, which help form blood vessels into an environment where “the cells are happy, so that they multiply, grow and start forming the blood vessel.”
The ultimate test was: When put on a bone, does the blood vessel actually connect with the blood vessel of the host? “In the lab, we can keep the graft alive by giving it nutrients, but once we put it on the bone it needs its nutrients from the host,” Karande said.
Learn More About: Researchers 3D Print on Skin for Breakthrough Applications
The skin the Rensselaer team printed was grafted onto a special type of mouse by the Yale team. Soon the skin began to communicate and connect with the mouse’s own vessels. “The integration with the wound, the development of the blood vessel, the connections with the host vessels, the maturation of the tissue in the wound was for us a big step forward,” he said, explaining the process in a short video.
Karande said the biggest challenge was actually optimizing the system as a whole after optimizing steps along the way. Everything was equally important: From harvesting cells from patients to isolating them, having them maintain their biological properties, and then getting all of these components to grow to a nice number of cells and cell density to make new components, then keeping the graft alive, making sure it is sterile, suturing it on the wound of an animal and even more.
“Each of these steps required a lot of trials. So it was incremental progress at each step but when you add up all those steps, you have a big advance,” he said.
The next big step will be working toward a universal prefabricated graft that will not be rejected by any patient’s immune system. Customizing a graft to each individual using their own harvested cells could take weeks or even longer—time that most patients needing a graft do not have.
To create a universal graft, researchers are gearing to work with CRISPR, a sophisticated gene editing technology. They will turn off those markers in graft’s cells, which tell the body the graft is a foreign object that should be rejected.
Editors' Pick: 3D Bioprinter Prints Healthy Skin onto Patients in Minutes
Additionally, long-term testing still needs to take place. The hope is that in the short term the graft will facilitate wound healing and provide protection by serving as a natural barrier. Then, with time, the body’s own cells will take over and repopulate the site with its own cells. Typically, human skin regenerates every 30 days.
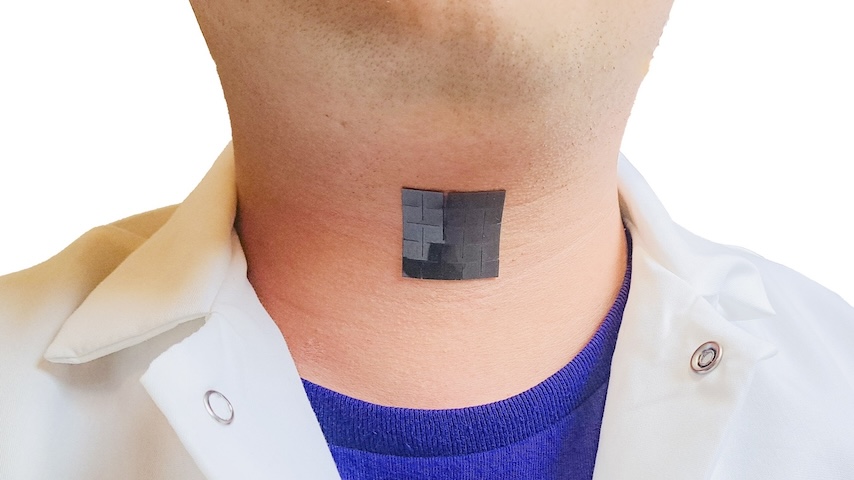
Currently, therapeutic interventions for treating any kind of skin injury, especially when small pieces of skin are effected—such as pressure ulcers, diabetic patients, or gun victims—involve harvesting skin from another location on the body and grafting it. This creates another wound that needs to be addressed.
There are a few clinical products on the market that contain some growth factors, but they are essentially what Karande calls “fancy Band-Aids,” because they prevent wound exposure to the environment. Without any blood and nutrients in the graft, it will eventually fall off.
For burn patients, still more work needs to be done to deal with the lost nerve and vascular endings.
“As engineers working to recreate biology, we’ve always appreciated and been aware of the fact that biology is far more complex than the simple systems we make in the lab,” Karande said. “We were pleasantly surprised to find that, once we start approaching that complexity, biology takes over and starts getting closer and closer to what exists in nature.”
Nancy S. Giges is a technology writer based in New York.
Register Today for AM Medical: May 27–28, 2020 in Minneapolis, MN
In the most recent development discussed in an article in Tissue Engineering, Karande, an associate professor of chemical and biological engineering at Rensselaer Polytechnic Institute, and the team in his lab at Rensselaer, collaborating with Yale School of Medicine, have developed a way to use 3D printing to incorporate blood vessels into the living skin they produce. “That was a big breakthrough,” Karande said.
Skin Bioprinting
Within the past decade, 3D bioprinting has actually played a starring role in advancing the field of skin engineering. Karande published one of the first papers in the field showing that researchers could make a bio-ink from two types of living human cells and use a 3D printer to produce a skin-like structure. The traditional procedure for making skin was to take cells, mix them up with collagen, and spread them in thin layers.
“You might liken it to spreading jam on a piece of bread in layers,” he said, adding that it’s very hard to do so manually, because you are working with tens or hundreds of microns that need to be close to the other cells for normal interaction.
You May Also Like: Artificial and 3D-Printed Skin Advances for Robots, Humans
3D printing has allowed precise placement and arrangement of the cells in three dimensions on a very small scale—this material that can be 10 times thinner than a human hair. “That’s been the big advancement that 3D printing has allowed in soft tissue engineering,” Karande said.
Although this was a “big advancement,” a few years ago the team realized that for the grafts to survive on patients, blood vessels are very critical. At that time a lot of work was being done on combining endothelial and other cells to try to form blood vessels, but the available methods weren’t working.
Incorporating Blood Vessels
Karande’s team decided to try putting cells, which help form blood vessels into an environment where “the cells are happy, so that they multiply, grow and start forming the blood vessel.”
The ultimate test was: When put on a bone, does the blood vessel actually connect with the blood vessel of the host? “In the lab, we can keep the graft alive by giving it nutrients, but once we put it on the bone it needs its nutrients from the host,” Karande said.
Learn More About: Researchers 3D Print on Skin for Breakthrough Applications
The skin the Rensselaer team printed was grafted onto a special type of mouse by the Yale team. Soon the skin began to communicate and connect with the mouse’s own vessels. “The integration with the wound, the development of the blood vessel, the connections with the host vessels, the maturation of the tissue in the wound was for us a big step forward,” he said, explaining the process in a short video.
Karande said the biggest challenge was actually optimizing the system as a whole after optimizing steps along the way. Everything was equally important: From harvesting cells from patients to isolating them, having them maintain their biological properties, and then getting all of these components to grow to a nice number of cells and cell density to make new components, then keeping the graft alive, making sure it is sterile, suturing it on the wound of an animal and even more.
“Each of these steps required a lot of trials. So it was incremental progress at each step but when you add up all those steps, you have a big advance,” he said.
CRISPR for a Better Skin Graft
The next big step will be working toward a universal prefabricated graft that will not be rejected by any patient’s immune system. Customizing a graft to each individual using their own harvested cells could take weeks or even longer—time that most patients needing a graft do not have.
To create a universal graft, researchers are gearing to work with CRISPR, a sophisticated gene editing technology. They will turn off those markers in graft’s cells, which tell the body the graft is a foreign object that should be rejected.
Editors' Pick: 3D Bioprinter Prints Healthy Skin onto Patients in Minutes
Additionally, long-term testing still needs to take place. The hope is that in the short term the graft will facilitate wound healing and provide protection by serving as a natural barrier. Then, with time, the body’s own cells will take over and repopulate the site with its own cells. Typically, human skin regenerates every 30 days.
Currently, therapeutic interventions for treating any kind of skin injury, especially when small pieces of skin are effected—such as pressure ulcers, diabetic patients, or gun victims—involve harvesting skin from another location on the body and grafting it. This creates another wound that needs to be addressed.
There are a few clinical products on the market that contain some growth factors, but they are essentially what Karande calls “fancy Band-Aids,” because they prevent wound exposure to the environment. Without any blood and nutrients in the graft, it will eventually fall off.
For burn patients, still more work needs to be done to deal with the lost nerve and vascular endings.
“As engineers working to recreate biology, we’ve always appreciated and been aware of the fact that biology is far more complex than the simple systems we make in the lab,” Karande said. “We were pleasantly surprised to find that, once we start approaching that complexity, biology takes over and starts getting closer and closer to what exists in nature.”
Nancy S. Giges is a technology writer based in New York.
Register Today for AM Medical: May 27–28, 2020 in Minneapolis, MN